Trending
Elections 2024
Jobs
- Audiologist Swellendam
- Head of Marketing Johannesburg
- Diagnostic Radiographer Cape Town
- Customer Service - UK - Work from Home Nationwide
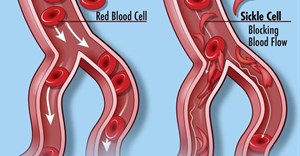
Building a sickle cell disease registry in Africa

Although several effective interventions and therapies have been established, these are largely available in high income countries resulting in a major need for research to develop new, effective SCD therapies and healthcare interventions. The establishment of newborn screening and comprehensive care have led to an increase in the life expectancy of adults in high income countries to the fifth and sixth decades.
In 2017, the National Institutes of Health’s National Heart, Lung, and Blood Institute (NHLBI) took a bold move towards addressing SCD in Africa by funding the establishment of the SickleInAfrica Consortium which aimed to establish a registry of over 13,000 SCD patients in Africa and to develop standards of care for this condition amongst other capacity development related research and healthcare aims.
The consortium began as a partnership between the Sickle Africa Data Coordinating Centre (SADaCC) and the Sickle Pan African Research Consortium (SPARCo).
SADaCC was established at the University of Cape Town (UCT) to provide administrative, data management and analyses, ethical and legal, and other support to the consortium.
Data
According to SADaCC principal investigator Professor Ambroise Wonkam, the aim of SickleInAfrica is “developing robust data infrastructure for both research and clinical care including setting newborn screening programmes for SCD, and implementation of a comprehensive care including penicillin prophylaxis by developing research around the quality of life people living with SCD.”
The life expectancy of patients with SCD has improved considerably since 1960, when Sir John Dacie described SCD as “essentially a disease of childhood.” In his 1973 review based on autopsies, Dr Lemuel Diggs estimated a median survival of 14.3 years, with 20% of the deaths occurring in the first two years of life, one third occurring before the fifth year of life, half between five and 30 years of age, and one sixth after the age of 30.
However, even in high income countries such as the United States of America, mortality in adults living with SCD has not changed over the past four decades, due to end-stage debilitating cardiovascular complications associated with poor quality of life. Among those with sickle cell-hemoglobin C disease, the median age at death was 60 years for males and 68 years for females. Among adults with SCD, 18% of the deaths occurred in patients with overt organ failure, predominantly renal.
Mortality
Therefore, there is a need to address mortality and morbidity associated with SCD, not only in Africa, but across the globe. The consortium aims to establish multicentric prospective SCD cohorts in Africa to rigorously gather environmental and generic factors associated with the pathophysiology of SCD. And to develop and implement the outcomes of research that explores new therapeutic frontiers of SCD in Africa.
“I believe we will be able to achieve our vision of improving the quality of care and the lives of people living with SCD," he says.
According to Professor Julie Makani Makani, principal investigator of the SPARCo Centre “... the issue of equity and time, when you think about how long it’s been since SCD was first described, more than 110 years ago, and you look at the individuals with SCD in our countries, we have to address the fact that, we have to make sure that they have access to care that they should be receiving, and this is the whole ethos of SPARCo and SADaCC to be able to build infrastructure to optimise standards of care; to identify the research questions that are important and; to be able to conduct research in our setting to see what and where and how we can provide care.”
Standard of care guidelines
During the past five years, the consortium has successfully enhanced and developed research capacity across the sites, evident in the recruitment of over 13,000 patients into their registry – making this the largest SCD patient database globally.
Other key outputs from this phase of SickleInAfrica include standards of care guidelines, the Sickle Cell Disease Ontology, big data analytics skills, community and public engagement materials including videos, and ethical and legal guidelines and templates.
Based on the success of Phase 1 of SickleInAfrica, the NHLBI recently awarded grants to support SickleInAfrica for another five years and Phase 2 was recently launched in a virtual event.
SickleInAfrica plans to advance the SCD agenda in Africa towards improving patient care and quality of life by leveraging the established cohort of over 13,000 patients with more than R218m.